
In the past there was little question about who owned the HIT Strategic Plan – the Chief Information Officer (CIO). That has changed in many organizations. Organizations are creating new C-suite officer roles – chief data and analytics (CDAO), chief digital officer (CDO or CDIO), chief data officer (CDO), chief information and innovation officer (CIIO), chief AI officer (CAIO). Strategic initiatives, once the purview of CIOs, are being led by many of these individuals in their new roles. Why have the CIO roles been reassigned?
One reason is that traditional CIOs have not redefined their roles quickly enough to take on responsibilities which should be owned, overseen, or coordinated by them. Another reason is that other members of the C-Suite have thought of the CIO as a technologist, not as a businessperson. The third reason is that CIOs have created their own strategic plans separately and apart from the enterprise strategic plan.
To reverse this trend, CIOs must think strategically and function tactically as business leaders ensuring their strategic initiatives and plans are fully aligned with and incorporated into the enterprise strategic plan. Rather than displacing the other roles, it would make more sense to set up an Office of the CIO with all the other IT-adjacent chiefs as participants with either a direct or dotted line relationship to the CIO. The overall HIT strategy should have elements in support of all these areas.
Regardless of who owns it, HIT strategic planning is not only relevant but essential. I’ll explain shortly why the CIO should champion efforts to initiate or lead the change.
Almost all healthcare delivery system’s strategic plans are developed using traditional planning horizons that cannot and do not support the rapidly evolving digital health ecosystem.
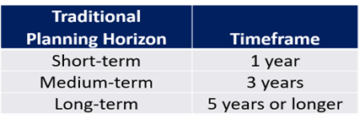
In recent years, many forward-thinking providers started their journey to function as digital enterprises. Some are just beginning. I searched the internet without success for new digital health inspired strategic planning timeframes. I inferred that no organizations (or too few to report) have migrated away from the traditional planning timeframe above. Timeframes for strategic planning dramatically impact the planning process which directly affects financial and operating (tactical) plans.
There is opportunity to redefine the timeframes. Existing timeframes should be shortened and a new one – immediate – should be added. The factors that support the immediate timeframe are the prevalence of mobile apps, other digital consumer-oriented experiences which have raised expectations, and the rapid adoption of AI.
I would suggest that the new approach to enterprise strategic planning be modified to:
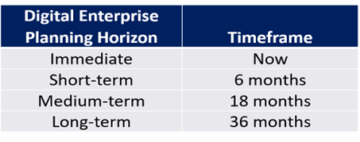
Though some organizations have adjusted their budget planning cycles to account for a faster pace of change, a new framework does not require organizations to make that change. It does, however, suggest the need for an increased sense of urgency and embracing incrementalism to achieve success in steps, not huge leaps. We all must think of patients and families as consumers, which makes this new approach even more relevant.
To survive and prosper, every provider organization must become a digital enterprise and every CIO must think about how to use IT holistically – clinically, fiscally, and administratively – to meet the evolving needs and challenges facing provider enterprises.
This new approach to HIT strategic planning has many benefits.
• Provider organizations operate at the nexus of 2 of the most very rapidly evolving and changing industries – healthcare and technology. Shorter timeframes can help create more adaptable organizations. I paraphrase a quote attributed but not said by Darwin, “it is not the most intellectual nor the strongest of the species that survives; but the species…that is best able to adapt and adjust to the changing environment in which it finds itself.”
• Except for facility projects and a few other exceptions, shorter timeframes should encourage planners and participants to identify incremental improvements that can help sustain enthusiasm. Benefits from incremental steps in projects will be realized sooner.
• Rapid advancements in HIT and clinical practice necessitates continuous strategic planning to integrate newer, more efficient, effective, and equitable solutions into operations. Ideally, clinical and technological advances and best practices could be deployed more quickly.
• Demand for IT resources will far exceed the supply which may provide the incentive to revisit and ensure organizations have strong, yet lightweight, demand management and data governance in place.
• Local, regional, state, and national regulatory bodies are more active than ever. More frequent strategic planning allows those affected to address the impacts – positive and negative – on existing operations in a timelier manner.
• Given the data “tsunami” upon us and the availability of new data elements (e.g., Social Determinants of Health) and more comprehensive data sources, updating a strategic plan and its supporting data management plan more often should provide better fuel for analytics engines which can improve all types of decision-making. More and better insights gained from the analytics will improve all operations.
• Perhaps the greatest challenge and the biggest opportunity is how to improve coordination of care among and between all providers in the care continuum for the sake of the patients and their families. Embracing incrementalism means that strategic plans can focus on continuous improvements far sooner than is done now. Rapid app development and deployment have an advantage over traditional application practices. Incremental successes have a favorable impact on all elements of the Quintuple Aim but particularly on satisfaction.
There are some drawbacks.
• Change is usually good; transitions, usually very difficult. Incrementalism implies multiple transitions. People do not always transition from old to new at the same pace. It is likely the laggards will be upset. You’ll need excellent change managers in place. Developing a culture that embraces change will not be easy.
• Communication can be challenging. A faster strategic planning process requires more, better, and easier to understand communications. Done well, a strong communication plan must be delivered in modes that address all types of learners and should make it easy for every stakeholder to answer two questions, “Why are they doing that?” and “What’s in it for me?”
To thrive, healthcare organizations must embrace a culture of rapid adaptation, fueled by an aggressive pursuit of innovation. This requires a fundamental shift in strategic planning – one that aligns with the rapid pace of clinical and technological advancement. By shortening planning horizons and prioritizing incremental improvements, healthcare providers can position themselves at the forefront of digital transformation.
The challenges are real, but the rewards are immense. By adopting a new approach to HIT strategic planning, organizations can enhance patient care, improve operational efficiency, create a more satisfying environment for patients, family, and providers, and unlock the full potential of data-driven insights. The time for incremental steps is now. The future of healthcare depends on it.

1 comment
David,
well stated and I completely agree. Both technology and healthcare are evolving too rapidly. Investing in a 5+ year long range plan is no longer prudent as rapid market changes decrease the predictability of organizations’ requirements far into the future.
I think that you are seeing a lot of these new sexy “C” level positions because important initiatives are not being delivered quickly enough by IT. I see CDataOs where Data and Analytics initiatives are not leveraged fast enough, and CDigitalOs where direct to consumer (patient) initiatives are lagging. Today’s CIO has a lot more on their plate then in the past. If they are not restructuring IT and their relationship with their business piers, they will get stuck spending a lot of calories keeping that old cardiology system alive – even though it has little organizational value.
I advise my clients to bake their organizational strategy into the guiding principles for decision making and prioritization and that all business and IT leaders agree and adhere to these principles. These principles should be grounded in the mission and vision of the organization. I find it unlikely that the company will revise their mission every 5 years. This way, when market changes introduce new business opportunities leadership can quickly make decisions that align with a broader and longer strategy and align with the mission. This positions organizations to be more Business Agile.
Naturally, IT must rethink how they deliver services and solutions to align with Business Agility. I have been working with several organizations to implement Lean Agile development frameworks …IT Agility. Aligning IT staff and workflow to enable an ability to pivot based on business priority without compromising productivity levels. Getting away from the practice of funding long-term projects and measuring IT by their ability to deliver on-time and on-budget, and pivot to a mentality of funding IT and measuring it by the value derived. PMOs must evolve to VMOs if they are going to be successful in a rapid change market.
Sounds straight forward and simple, but it is surprising how difficult it is to get health systems into a mode of agility. They want to be agile, and they want to shorten time-to-value, but they can not let go of the habit of planning long drawn-out projects that are all inclusive of every potential desirable option and feature – and having 50 active projects in progress at the same time. If a project takes longer than 18months to begin recognizing value, it had typically missed the market. Better to break traditional projects into shorter minimum viable features, sort these features by time and value, focus on the highest value features first, and limit the amount of concurrent work in progress (WIP).
It is still a struggle though. I continue to have business leaders ask, “when will my project be complete?”. The real answer is that it may never be “complete” because some components of your project have very little value to the organization. However, the high value components (features) of the project will go-live faster – based on the agreed upon principles that we are using for decision making. The bigger the ship, the harder it is to change course.
Best to you, Sir.